
Atlantic Oral Surgery and Implant Center
Experts for all your family needs.

Wisdom Teeth Removal?
Choose the Experts.

Restore Your Smile
With Dental Implants.
Welcome
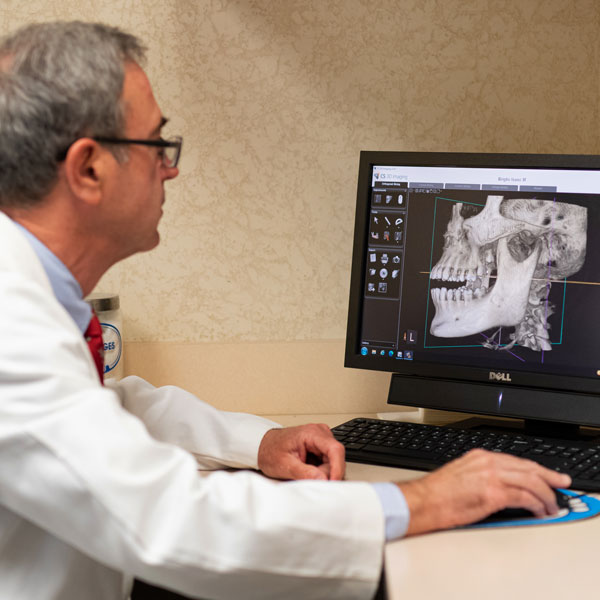
Atlantic Oral Surgery and Implant Center
We believe that a doctor and patient become a team for treating an individual’s oral and maxillofacial needs. Dr. Wallen spends most of his time listening to understand your concerns and responding with the best treatment options for you. With the help of our professional staff, he also follows up to make sure that pain is relieved, problems are resolved, and your oral health improves.
We also want our patients to be informed about problems and treatments requiring oral surgery because informed patients make better decisions about their health and well-being. That is why we’ve included an extensive section on this website covering the full array of topics associated with oral and maxillofacial diagnoses and treatments. We encourage you to look through these pages whenever you have an interest or concern about oral surgery.
We also know that convenience in the Myrtle Beach area is important to your selection of an oral and maxillofacial dentist. In these web pages, you’ll find information about Dr. Wallen’s office, including our Myrtle Beach location, maps, directions, hours, insurance policies, and appointment scheduling. Please feel free to contact us with any questions you have or to request an appointment. We hope you’ll find our practice offers the accessibility and personal commitment you look for from an Oral Surgeon.
Tooth Extraction
While tooth extraction may be a little scary, you are in good hands with Atlantic Oral Surgery and Implant Center. Whether you’ve been referred to us by your family dentist or you’re just now finding us online, we’ll make sure your procedure is as comfortable as possible. We specialize in all types of extractions and have multiple options of comfortable anesthesia techniques to make your extraction as comfortable and safe as possible.

Contact Us
Whichever appointment you need, the first step towards recovery and a beautiful smile is scheduling your appointment. Contact our office today by giving us a call or completing the appointment request form. From there, one of our friendly staff members will reach out to you and coordinate your appointment. Please refrain from using this form to communicate your private health information. We will cover these topics while you’re in our office.
Atlantic Oral Surgery and Implant Center
Address
1200 48th Ave N, Suite 101
Myrtle Beach, SC 29577
Phone
843-449-4993
Hours of Operation
Monday: 7:00 AM – 4:30 PM
Tuesday: 7:00 AM – 4:30 PM
Wednesday: 7:00 AM – 4:30 PM
Thursday: 7:00 AM – 4:30 PM
Friday: 7:00 AM – 3:00 PM
1200 48th Ave N # 101, Myrtle Beach, SC 29577, USA



